Diabetes is no longer a condition limited to later life—it’s rising rapidly among young adults, and many people don’t realize they’re already on the metabolic edge. The good news? Pre-diabetes does not have to progress to diabetes. With the right interventions—stress management, optimized nutrition, smart fasting windows, and targeted nutrient support—you can rewrite your metabolic future.
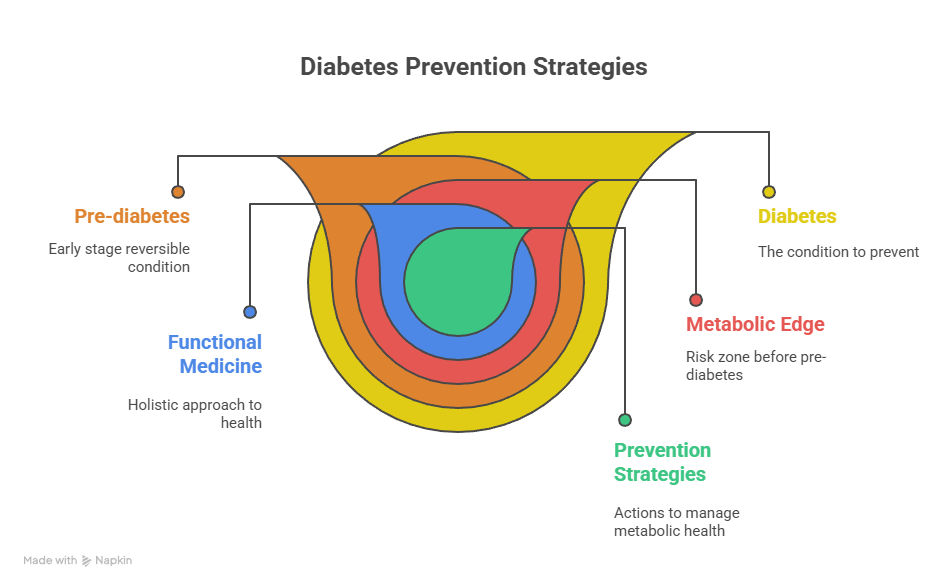
This guide explores five major pillars of prevention through the lens of a functional medicine doctor and evidence-based strategies that help halt or reverse pre-diabetes.
1. Understanding Pre-Diabetes and How to Prevent Its Progression
What is Pre-Diabetes?
Pre-diabetes is a state where blood sugar is higher than normal—but not high enough for type 2 diabetes (T2D). It’s a metabolic warning light. The CDC estimates 1 in 3 adults have pre-diabetes, and over 80% don’t know it.
Why It Matters
People with pre-diabetes have a high risk of progressing to T2D—somewhere between 5–10% per year. But the encouraging news is that reversion back to healthy glucose levels is possible. Lifestyle, nutrient status, and metabolic balance make a tremendous difference.
Risk Factors for Progression
- Overweight/obesity (especially belly fat)
- Low physical activity
- High-glycemic or processed diet
- Insulin resistance
- Fatty liver
- Chronic inflammation, poor sleep, high stress
- Age & genetics
Why Early Prevention Matters
Once full diabetes develops, complications escalate. But when you intervene early, you can delay or completely prevent diabetes onset.
A Functional Medicine Approach
A functional medicine doctor views pre-diabetes as a multi-system metabolic imbalance involving hormones, gut health, inflammation, stress, toxin exposure, circadian rhythm, and nutrition. Lab testing may include:
- Glucose, insulin, HOMA-IR
- Fatty liver markers
- Gut and microbiome testing
- Inflammatory markers
- Thyroid & adrenal hormones
- Nutrient status (Mg, B12, zinc, vitamin D)
Once root causes are identified, a personalized prevention plan is built—addressing diet, gut health, movement, sleep, detoxification, and stress resilience. Many patients not only prevent diabetes but return to normal metabolic health when guided by a functional medicine doctor.
2. The Impact of Stress on Blood Sugar Levels
How Stress Affects Glucose
Stress activates the HPA axis, raising cortisol and adrenaline. These hormones:
- Increase glucose production
- Lower insulin sensitivity
- Promote fat storage (especially around the abdomen)
- Disrupt sleep, driving cravings and overeating
Stress & Diabetes Risk
Studies consistently link chronic stress, anxiety, and depression with higher diabetes risk—even independent of body weight or diet.
Stress Management Strategies
- Meditation, breathwork, yoga, tai chi
- 7–9 hours of restorative sleep
- Walking, stretching, daily movement
- Social connection, therapy, journaling
- Adaptogenic herbs (under supervision)
- Better time boundaries and lifestyle balance
A functional medicine doctor carefully evaluates stress physiology because stress is one of the major overlooked drivers of insulin resistance.
3. Trend Sound: Current Eating & Lifestyle Trends Affecting Diabetes Risk
Time-Restricted Eating & Chrono-Nutrition
Research shows that eating earlier in the day supports better metabolic function. Early Time-Restricted Eating (8 am–4 pm) improves glucose and lipid metabolism even when calories are the same.
Intermittent Fasting
A rising trend supported by science for improving:
- Insulin sensitivity
- Liver fat
- Glucose control
- Weight management
Sedentary Lifestyles
Even active people suffer from “sitting disease.” Short movement breaks, post-meal walks, and standing desks help improve metabolic health.
Ultra-Processed Food Consumption
Global intake of processed foods continues to rise, contributing to high glycemic load, poor insulin function, and overeating.
Sleep Disruption
Poor sleep and irregular schedules increase risk of metabolic dysfunction.
A functional medicine strategy integrates lifestyle architecture—sleep, movement, nutrient density, circadian rhythms, and reduced processed foods—to reduce diabetes risk proactively.
4. The Benefits of Intermittent Fasting for Diabetes Management
Intermittent fasting (IF) is now scientifically recognized as a powerful metabolic tool.
Key Research Findings
- A 2024 clinical trial found a 5:2 fasting method outperformed metformin and empagliflozin in reducing HbA1c.
- Meta-analyses show IF improves glucose, insulin resistance, weight, and liver fat.
- IF may prevent progression from pre-diabetes to diabetes.
Why IF Works
- Reduces insulin levels & improves sensitivity
- Promotes fat burning and metabolic flexibility
- Stimulates autophagy (cellular cleanup)
- Supports circadian-aligned eating
- Reduces liver fat
Practical Tips
- Popular methods: 16:8, 14:10, 5:2, early eating windows
- Start slowly: begin with 12 hours fasting
- Eat nutrient-dense whole foods
- Avoid late-night eating
- Monitor glucose if on medication
IF must be customized—ideally guided by a functional medicine doctor—especially for people on glucose-lowering medications.
5. IV Therapy for Diabetes: Supporting Nutrient Deficiencies
Many people with pre-diabetes or T2D have nutrient deficiencies that impair metabolic health.
Why Nutrients Matter
Magnesium, chromium, zinc, vitamins D, B12, and antioxidants support:
- Insulin signaling
- Glucose transport
- Mitochondrial function
- Beta-cell health
- Detoxification and inflammation control
Benefits of IV Therapy
- Rapid correction of deficiencies
- Higher absorption vs. oral supplements
- Personalized nutrient blends based on lab testing
- Support mitochondrial and cellular repair
- Enhance antioxidant capacity (e.g., glutathione)
Important Considerations
- Not a replacement for lifestyle changes
- Best for people with malabsorption or documented deficiencies
- Requires medical monitoring
- Works best as part of a comprehensive prevention strategy
A functional medicine doctor uses IV therapy strategically to accelerate metabolic repair in people at risk for diabetes.
Conclusion & Call to Action
Preventing diabetes is about strategic, early, whole-body intervention—not waiting until blood sugar becomes uncontrollable. When you apply:
- Stress reduction
- Circadian-aligned nutrition
- Intermittent fasting
- Nutrient-rich whole foods
- Targeted IV nutrient therapy
- Guidance from a functional medicine doctor
—you shift from metabolic risk to metabolic resilience.
If you have borderline HbA1c, elevated fasting glucose, or high insulin levels, now is the time to act.👉 Book your personalized metabolic prevention consultation at ivitalitymd.com
Take control of your metabolic health today and protect your long-term vitality.
Visit us for more info:- https://www.facebook.com/IVitalityMD/